An outline of the services we offer.
If you are uncertain as to how we might help you, do make contact and ask.
Hip pain
In younger patients, an underlying hip deformity or joint problem can cause one or more of the following symptoms:
- Activity-related hip pain, (especially in the front of the hip, groin region, or even knee)
- Discomfort with prolonged walking, running, pivoting, sitting, hip flexion motion, or various other impact activities
- A soft tissue injury around the hip typically responds to standard nonsurgical treatment in 6 to 8 weeks. If symptoms last 3 to 4 months, a hip joint problem may be the cause
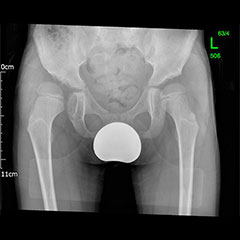
DDH (Hip Dysplasia)
Developmental dysplasia of the hip (DDH) is the most common paediatric hip condition. Abnormal hip development in the womb leads to a joint that can be unstable or even dislocated at birth. Children may present with a leg length discrepancy, restricted abduction, abnormal gait (walking) or even signs of instability. This can be missed, especially if both sides are affected. Earlier treatment is less invasive and more effective.

Perthes' Disease
A serious condition of the hip caused by transient compromise of the blood supply to the joint. Typically affects boys aged 4-8 years and can cause pain and restricted mobility throughout childhood. Some children may benefit from surgery but decision-making is complex and indications vary between surgeons. In Bristol we are represented on an important group of international surgeons aiming to improve our understanding and treatment of the condition.
Young Adult Hip Preservation Surgery
'Hip Preservation Surgery' is a non-specific term that refers to surgical methods aimed at preserving your own hip and essentially avoiding a hip replacement. Ideally, in order to be a candidate for this type of surgery, the vast majority of the cartilage in the joint has to still be intact. This means that, ideally, the hip shouldn't have any arthritis, or at the very least minor wear. Unfortunately, in some patients, too much cartilage has been damaged. In these cases, hip preservation is not an option and a consultation with a hip replacement surgeon is required.


Osteotomies around the hip
Surgeries on the hip socket side are called ‘acetabular osteotomies’ or ‘pelvic osteotomies’ and of these the PAO (periacetabular osteotomy) is the most common type for young adults. This is also called the Ganz or Bernese osteotomy because it was developed by Professor Ganz in Berne, Switzerland. Surgery on the top of the thigh bone (just below the hip joint on the ball side of the joint) are called ‘femoral osteotomies’. These may be varus (tilting the hip in) or valgus (tilting the hip out), or an isolated trochanteric procedure, depending on the precise aim of surgery. The conditions that can be treated with osteotomies around the hip are as follows:
- Hip Dysplasia
- Consequence of Paediatric Hip Disease
- Slipped Upper Femoral Epiphysis
- Perthes’ Disease
- Avascular Necrosis
- Transverse Plane Mal-Alignment in the Femur (Miserable Mal-Alignment)
Knee pain
Knee pain is common in physically active adolescents, who can sometimes experience pain in the front and centre of the knee, usually underneath the kneecap (patella). Adolescent anterior knee pain is not usually caused by an abnormality within the knee, but by overuse or a training routine that does not include adequate stretching or strengthening exercises. In most cases, simple measures like rest, over-the-counter medication and strengthening exercises relieve anterior knee pain and allow the young athlete to return to his or her favourite sports.


Growth related pain
All the major joints in children have adjacent plates of growth cartilage which are liable to strain from overuse, particularly where muscles insert into them. Continued traction from the quadriceps can lead to a repetitive injury to the growth plate causing pain and swelling. Around the knee this can be called Osgood-Schlatter's, Sinding-Larsen-Johansson syndrome or Jumper's knee depending on the site of the pathology. Rapid growth associated with the adolescent growth spurt, regular high impact sports such as repetitive running, jumping, football and gymnastics are all implicated in its aetiology. History and examination are sufficient to form a clinical diagnosis; X-rays are usually normal. Treatment usually involves rest and physiotherapy with surgery rarely indicated.
Sports Injuries
If knee pain is associated with swelling or mechanical symptoms, it may be a sign of other pathology such as OCD (osteochondritis dissecans) or a meniscal injury. OCD occurs when a loose piece of bone and articular cartilage separates from the end of the joint. This piece may stay in place and cause pain or fall into the joint space, causing mechanical symptoms and instability. Children usually between the ages of 10 and 20 experience pain, which is often poorly localised and associated with activity. Swelling may be present, and particularly in a case of an unstable piece, the patient may describe mechanical symptoms such as locking or catching. The outlook is favourable if the skeleton is still growing, but large or unstable lesions may require enforced rest or even surgery. An MRI scan will usually be required to characterise these defects.
Immediate and marked swelling of the knee after injury may indicate a torn cartilage or ligament and should be investigated promptly.
Injuries to the anterior cruciate ligament are also being seen in increasingly younger children, although those under the age of 12 remain more likely to pull out the bone insertion rather than rupturing the ligament itself. Fixation or reconstruction requires careful consideration of the nearby growth plates which contribute the majority of leg growth.
Ankle Pain
Ankle sprains are common in children and young adults. While the vast majority settle within 2 weeks, some patients can experience persistent pain or a feeling of instability within the ankle. Investigation may involve X-rays or an MRI scan. Management is usually physiotherapy in the first instance, but surgery may be indicated in patients with persistent instability.
Flat feet
The majority of children between 1 and 5 years of age have flat feet. This is part of normal development and over 95 percent of children grow out of their flat feet and develop a normal arch. The other 5 percent continue to have flat feet, but only a small number will ever have a problem. Most children with a persistent flat foot participate in physical activities, including competitive sports, and experience no pain or other symptoms. On rare occasions, there can be an underlying problem, and it is important to distinguish between physiological (normal) flat foot and a 'pathologic' (abnormal) flat foot.
Although there is no indication for treatment in a physiological painless flat foot, a pathological flat foot may require further investigation and treatment depending on the underlying cause. An easy way of determining what type of flat foot your child has is to get them to stand on tip toes. If the arch of the foot reconstitutes, this implies that the foot is supple and the deformity physiological.
Hallux Valgus (Bunions)
Bunions can occur in children and adults. Juvenile hallux valgus is the name for a bunion that develops during childhood. No one knows with certainty why juvenile hallux valgus occurs.
Juvenile hallux valgus causes a bump on the inside of the foot at the base of the great toe and some children are very sore around it.
Children and teens with bunions should wear shoes with a wide toe box and low heels so they don't put too much pressure on the bump or make the condition worse. Orthotics and physiotherapy may help, particularly in children with flat feet.
Surgery should only be considered for children who have persistent, significant pain which gets in the way of activities, even after trying non-surgical treatment.
There are several surgical procedures used to correct this deformity; much of the surgical decision making depends on how the foot looks on physical exam and x-ray.


Sever's Disease
Sever's disease is pain over the insertion of the Achilles tendon. It is usually unilateral but can be bilateral in some cases. The pain is made worse by sporting or high impact activities and can commonly cause pain after prolonged walking. It is focally sore to palpation over the posterior heel and sometimes can swell in this area.
History and examination are sufficient to form a clinical diagnosis; X-rays are usually normal. Management includes, pain relief, ice packs, physiotherapy and occasionally splintage or orthotics
Curly toes
Curly toes are a common condition that affect infants and children. Although present from birth, the condition may become more apparent as your child begins to walk. It is most often noticed in the 3rd, 4th and especially 5th toes. Often, it is bilateral and there may be a family history of it. The toes curl under because the flexor tendons that bend the toes are too tight and pull one toe under the next, curling it towards the underside of the foot. In many children, curly toes do not cause any symptoms, however some may experience:
- Flattening or Thickening of the Toenails
- Pressure Sores or Blisters
- Difficulty Wearing Some Style of Shoes
- Pain or Discomfort
Treatment is usually conservative unless the patient becomes symptomatic, in which case the simplest solution is to perform an operation to divide the tight tendon. This operation is a day case procedure, with no need for a plaster cast. Patients are advised to wear a stiff-soled sandal for about 2 weeks after.
Club foot
A relatively common neonatal foot deformity managed almost universally now with the Ponseti technique of serial manipulation and casting. Some children will require a small procedure to release the heelcord at the end of the casting phase of the treatment. Others may suffer a later relapse and require a slightly more invasive procedure to transfer a tendon across the foot.
When children are starting to find their feet, there can be some rather obvious abnormalities in the way they walk. While many of these are quite common and correct themselves on their own, some can require medical assistance. The following can be considered normal variations of gait in children, and parents often look to specialist for advice:
- Toe Walking
- In-Toeing
- Internal Tibial Torsion
- Metatarsus Adductus
- Genu Varum (Bow Legs)
- Genu Valgum (Knock Knees)
CP (Cerebral Palsy)
Cerebral palsy results from an injury to the immature brain. Although the brain injury remains static, the effects on the limbs do alter over time. Patients with CP may suffer from spasticity (high muscle tone), weakness, and poor coordination. The severity of involvement and treatment needed is variable. However, the overriding treatment goal for those with cerebral palsy is to:
- Optimise Mobility
- Control Pain
- Maximise Independence
- Enhance Social and Peer Interactions
- Improve Quality of Life
The management of children with CP is multidisciplinary and can involve paediatricians, physiotherapists, orthotists, orthopaedic surgeons and many others.
The type of treatment we can offer as orthopaedic surgeons include
- Regular review (including patients who have had SDR)
- Combined appointments with physiotherapy
- Botulinum (Botox) Injections
- Tendon releases
Trauma
Our paediatric orthopaedics can identify your child's injury and treat them accordingly.
We are two of nine paediatric orthopaedic surgeons who work at the Bristol Royal Hospital for Children, which is the designated children's major trauma centre for South West England. Together, we treat all types of paediatric fractures and trauma from both Bristol and the South West.